IMPACT BLOG

Sasha is a Research Paramedic and Academic Support Lead who has worked for ambulance services in the UK and the Caribbean since 2002. She has completed an NHSE AHP Clinical Fellowship and is completing the IMPACT programme of research for a Doctor of Philosophy (DPhil) degree in Experimental Psychology with the University of Oxford. Sasha has been awarded an National Institute for Health and Care Research (NIHR) Doctoral Research Fellowship and an NHSE Stipend to support her DPhil and research.
Dr Jennifer Wild

Dr Wild is a Professorial Fellow at the University of Melbourne, a Professor of Experimental Psychology at the University of Oxford, a Consultant Clinical Psychologist, and NIHR Oxford Health BRC Senior Fellow. Her research focuses on the treatment and prevention of post-traumatic stress disorder (PTSD), social anxiety, and depression in emergency responders.
Any Concerns about this research
Please contact Sasha, Dr Wild or SWASFT’s Head of Research and Audit; Dr Sarah Black via email or via the SWASFT research team contact form
Overview
Research title
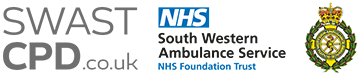
Integrating Mental health support in Partnership with Ambulance Clinicians, for enabling time-to-Talk (IMPACT): A co-produced multi-phase study [NIHR302983]
Aim
To investigate whether it is possible and acceptable to provide ambulance employees with dedicated time at work to enable them to think about work-related stress, as well as support needs, and determine whether this could help to improve employee well-being.
Research background
In comparison to the general population, ambulance employees are more likely to experience mental ill health and to die by suicide. Several patient complaints involve staff attitude and poor decision-making related to poor mental health. Causes of mental ill health are complex, although repeated stressful and traumatic events at work, typically experienced by ambulance employees, are known to increase the risk. If help is not sought for mental ill health, symptoms may get worse. This can affect physical health, result in a poor quality of life, and affect how staff perform at work. Mental well-being support is available, although ambulance employees report feeling too exhausted to look for help after work and the most vulnerable may not seek help at all. Staff also feel stigma and embarrassment about asking for help.
This step-by-step research plan will design the content of a dedicated space for employee well-being and will examine whether ambulance organisations can provide such a space in working hours. These sessions aim to help staff to talk about how their work makes them feel and whether any support is needed. This approach is in keeping with current compulsory training practices that ensure ambulance service employees are trained to manage patient needs.
Design and methods
The project will be built upon an ongoing review of all the available research about supporting ambulance staff well-being at work (under peer-review). The project team will then create the dedicated well-being session approach by:
- Using results from the ongoing review to work with staff and Patient and Public Involvement and Engagement (PPIE) groups to discuss what the research says and what they think the sessions should look like. A team of experts will then review this information and agree upon a finalised session. The session will include a set format to ensure safety and confidentiality, alongside updates about current wellbeing support options and signposting to support services as needed.
- Carrying out a small study involving 64 staff at 4 ambulance stations to see whether the session is acceptable and whether carrying out such a study is possible. We will aim to find out:
- willingness to get involved with sessions and complete feedback questionnaires;
- views about the usefulness of the session;
- whether sessions improve well-being;
- whether the study went as well as planned and if anything could have been done better;
- whether a larger scale trial could be undertaken.
PPIE / Service user involvement
Regular meetings with a reference group of 20 Ambulance staff (service users), 8 PPIE representatives and a professional consultation with 6 senior managers helped revise this research plan, based on previous research. Staff/manager suggestions include:
- Non-uniformed peer-to-peer rather than manager-led sessions, due to worries about organisational stigma.
- Video study updates as well as written summaries to aid information sharing, especially for minority group staff.
PPIE representatives improved the plan by:
- Recommending video conferencing for communication.
- Suggesting PPIE representatives share research findings as co-authors or co-presenters to highlight connections between patient care and staff well-being.
PPIE groups will help complete the research during regular meetings by reviewing the work as we go, sharing decision-making, whilst helping to interpret results and share findings.
Sharing findings
Results will be published in medicine and psychology journals and presented at conferences. Findings will be shared worldwide through the Association of Ambulance Chief Executives. Press releases, social media and a dedicated website will share results with staff, patients, and the public.
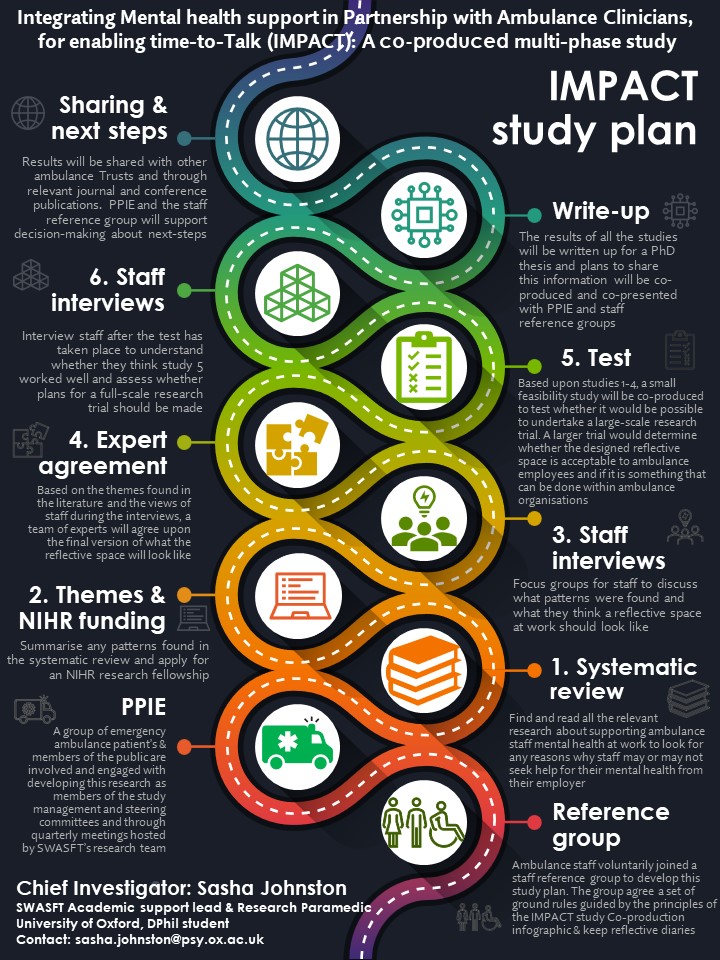
IMPACT Prototype
In terms of IMPACT development to date, a preliminary prototype model has been created from Sasha Johnston’s NIHR funded Master’s Degree research, literature searches and expert support. This model is framed by Clinical Supervision principles of providing a timed, structured, confidential, meeting at work. Mind’s Wellness Action Plan (WAP) (9 questions designed to support reflection about how to stay well at work) will be included to develop awareness of working style, stress triggers and responses. This will aid communication with a trained facilitator who will provide updates about available support and signposting if required. Initial findings suggest that session frequency of a minimum of once a year could align with current annual health and safety at work legislation and mandatory training, which would serve to normalise habits of mental health discourse and help-seeking into organisational culture. Session frequency could be modified to meet individual needs and connect the most vulnerable staff with support designed to help them.
Project Plan
Study 1 - Systematic Review
Study 2 - Qualitative Interviews
Consensus with Experts
Feasibility Trial
The feasibility trial will be designed with ambulance staff and patient and public contributors based upon information identified during the systematic review, qualitative interviews and expert opinion. The following logic model demonstrates what this process looks like:
Project Logic Model
Exclusion of Clinical Trials Unit (CTU) support rationale
The planned feasibility trial will be co-designed with ambulance employees and patient representatives. The Bristol Trials Centre have reviewed the proposed trial plan and agreed to support this project. However, the quote for CTU support was £50,000 and as:
- This is a PhD project
- Sasha’s academic supervisors are experienced in leading Clinical Trials
- South Western Ambulance Service’s research team are experienced at hosting and delivering Randomised Controlled Trials in the prehospital setting and fully support the project
- As a student Sasha will have access Oxford University’s Clinical Trials Research Unit for advice if needed
- Sasha will be undertaking a short course about Clinical Trials to supplement knowledge gained during her Masters in Clinical Research
On balance, it was decided that a spend of £50,000 on CTU fees could not be justified. It would therefore be reasonable to decline the CTU’s kind offer of support and utilise the resources available to assist the delivery of the IMPACT feasibility trial.
“Patients and the public are interested in being part of and getting involved with health and social care research for a variety of reasons. Most of all, not only are they hopeful of benefiting from more treatments but they also want to help others who are experiencing the same condition as them” – National Institute for Health and Care Research (NIHR)
IMPACT Public Contributor – Diana Frost

Why I am involved as a patient representative in NHS research
Hi my name is Diana and this picture was taken during a PPI meeting I attended in London. I got involved with working with Sasha for her IMPACT research as I want to help others have a better experience in their health and wellbeing journey, that I sometimes didn’t receive. I want to help health professionals realise that as a patient we do have a voice and our experience can help to improve services. For me this is also an opportunity to learn about health professionals and how research is so vital in giving data and methods which help to save money in the NHS. I can honestly say in the last nine years i’ve witnessed a greater improvement in standards and attitudes to PPI.
Why am I involved in the ambulance staff IMPACT study?
I believe our ambulance services do struggle with their mental health and wellbeing. As they are a patient first contact when an emergency arises, they also need support to talk and get counselling when needed, as many don’t. To have a dedicated space where they can talk and contact for help is vital, as during the pandemic they worked tirelessly and saw some very distressing and sad calls leaving behind family and them never getting to say goodbye to loved ones. This study is a step forward for our ambulance service and other health professionals working to give a backup for mental health & wellbeing which will result in a substantial amount of savings in sick leave and staff shortages.
IMPACT Public Contributor – Lynn Tatnell

Why I am involved as a patient representative in NHS research
I do PPI medical research because my daughters care throughout her 24 years was poor and unhelpful. She was not diagnosed although a few tests were undertaken. We were left to muddle through especially the last 5 years of undiagnosed Epilepsy. She died from SUDEP (Sudden Unexpected Death in Epilepsy) one Sunday night and even her care before being admitted to A&E was questionable. Nobody contacted me after her death which I find appalling to this day. I want better care for the public and patients, carers and their loved ones in the future and so I have volunteered with PenARC (Applied Research Collaboration, South West Peninsula) as a PenPEG (The Peninsula Public Engagement Group) member since 2009.
Why am I involved in the ambulance staff IMPACT study?
I am involved with the IMPACT study as I think its important for ambulance services to make sure their staff look after themselves and stay mentally well so they can make good decisions for patients.
SWASFT Patient Involvement in Research Group (PIRG)

A group of 8-10 patients, relatives and members of the public meet with SWASFT’s Research and Development team on a quarterly basis, to be updated about, discuss and get involved with SWASFT research.
IMPACT staff reference group – Olivia Bond

As this study focuses on ambulance staff (although enhancing patient care by improving ambulance staff wellbeing is the ultimate aim), it is important to include staff in developing this work as they are the ‘service user’ this research aims to help. A reference group of 20 staff have co-produced the IMPACT research plan and will be involved throughout the project in the interpretation, management and delivery of the research.
Participate in the IMPACT study
We are looking for ambulance service employees (in any job role) to join our reference group. The staff reference group share their perspectives and opinions to help to design and shape the research. Please contact sasha.johnston@swast.nhs.uk if you would like to ask any questions and/or would like to be added to the list.
Sasha was supported by SWASFT, NHSE, the NIHR Research Design Service, the University of Oxford, and employee and PPIE representatives to apply to the National Institute for Health and Care Research (NIHR) for a Doctoral Research Fellowship. Her application was successful and Sasha has been fully supported by the NIHR to undertake this programme of research since April 2023.
News Flash – April 2025
The International Journal for Environmental and Public Health Research have published our Systematic Review. Many thanks to all involved – https://www.mdpi.com/1660-4601/22/4/629.
Please visit the website ORCID (Open Researcher and Contributor Identifier) for a list of Sasha’s publications.